Alumnus physician leads emergency care at Sumner Regional
Dr. James Parnell works to bring more hope than fear to his staff during pandemic

JAMES PARNELL, MD, A 2006 LIPSCOMB GRADUATE, IS AN ATTENDING EMERGENCY PHYSICIAN AT SUMNER REGIONAL MEDICAL CENTER AND HAS LED LIPSCOMB’S MEDICAL MISSION TRIP TO CITY OF CHILDREN IN BAJA (PICTURED HERE) SINCE 2015.
Health care workers are working in a different world today than just two months ago. It’s now a world where patients can no longer see the face of the doctor caring for them. A world where one of the most important duties of a nurse is to hold the hand of a dying patient. A world where providing hope, in the face of rising fear, is a crucial management goal.
This is the world where James Parnell, MD, a 2006 Lipscomb graduate, is now working at the emergency room at Sumner Regional Medical Center, the largest hospital and the most experienced COVID-19 facility in Sumner County, 30 miles northeast of the Nashville metro area.
Parnell, an attending physician in the ER, is one of the many Lipscomb alumni now caring for COVID-19 patients across the nation during the current pandemic.
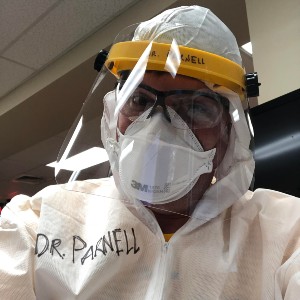
Dr. James Parnell
His emergency department had its own version of the COVID-19 surge on the weekend of March 29 when more than 90 patients from the Gallatin Center for Rehabilitation and Healing were sent to Sumner Regional after that facility was evacuated.
Fortunately, the hospital was well-prepared to handle such a crisis situation, said Parnell, noting that so far the facility has not experienced a shortage of personal protective equipment.
“Our hospital has been so well prepared for this. The plan has really worked well,” he said. “We are going to leave our (designated COVID-ER) open (after the end of the Safer-At-Home order) because it works as a containment area, so we don’t have a suspected COVID patient next to an appendicitis patient… It’s going to be a different world for a little while.”
On an average pre-pandemic day, Parnell said he would see about 20 to 25 people a day on an 8- to 12-hour shift in the 26-bed ER. Usual ailments in the ER are strokes, heart attacks, abdominal pain, broken bones and lacerations, he said. Two attending physicians would be available during most shifts.
At the start of the pandemic, Sumner Regional divided its ER into two: one for non-COVID emergencies and one for COVID and suspected-COVID cases only, with one physician overseeing each ER, he said.
Since then, the Sumner ER has experienced the same strange phenomenon that most Nashville health care facilities are experiencing during the pandemic: a drop-off in non-COVID emergency cases. Almost all the ER cases are now COVID-related, Parnell said.
Doctors and nurses in the COVID ER wear the full “bunny suit” and N-95 masks, covering their bodies and faces all day. “The first couple of hours you are OK in it, and then you start getting sweaty, and you get pressure areas on your head,” he said.
Hospital employees are going in just to hold the hands of people who are dying because we don’t want them to die alone... There has been a lot of Jesus’ spirit that I have felt at this time. —
In addition, the PPE, which covers up facial expressions, sometimes makes it hard to bring the personal side of medicine to patients who are already in a very lonely situation, as visitors are not allowed in the hospital at this time, Parnell said.
“That is one area where I have seen God working,” Parnell said of the obstacles to personal attention. “There are people in the ER, nurses and scribes, who are actively using FaceTime, so patients can say good-bye to their families or for families to call in and say, ‘I’m OK.’
“Hospital employees are going in just to hold the hands of people who are dying because we don’t want them to die alone. They are passing them on to Jesus on the other side. There has been a lot of Jesus’ spirit that I have felt at this time.”
Early in the pandemic, Sumner Regional also instituted a procedure for drive-through testing and treatments for patients who have COVID symptoms but don’t want to come inside the hospital because they are not sure if it is COVID, the flu or a cold, Parnell said. He uses an iPad to diagnose and treat patients from inside the hospital.

Parnell is also the leader of Lipscomb's medical mission trip to Baja, Mexico. Thanks to supplies transported to Baja in previous years, dentists and doctors in Mexico were recently able to receive N-95 masks and gowns.
“We were expecting a huge surge of patients, so we thought about how to help worried people while keeping them away from the COVID patients,” he said. “(We considered) how do we move them through efficiently while saving the hospital beds for those who need them? The plan has worked incredibly well.”
Since Tennessee’s Safer-At-Home order went into effect, the hospital has not seen a stretch like the Gallatin nursing home evacuation weekend, said Parnell, who was one of the doctors who urged the governor to enact the quarantine order earlier this month.
Many patients are now using telemedicine to deal with the daily emergencies of life, such as poison ivy, urinary tract infections or pink eye, Parnell said. He has been providing care through telemedicine for some time, so he’s pretty comfortable dealing with patients through the technology, he said.
“I feel like this has become a ministry in itself, being able to talk people through the process, describing symptoms they need to watch out for and the process to follow to get tested,” he said. “In mid-March we had a huge surge of telemedicine calls and mostly it was people simply asking, ‘What do I do?’
I have started playing worship music on my headphones, just to hear God’s promises in my head. —
“It’s a scary time to live in this paradox, and I ask myself, ‘How do I help?’ God has blessed me with skills and ability to care for patients, so I have great peace in that. I have to trust that He has me where he wants me to be, and you can’t dwell on the negative stories (you hear about health care workers suffering from COVID).
“All you hear about is COVID, COVID, COVID, but it’s your job to also take care of everything else that keeps happening. You have to filter out the COVID noise, and that is one of the hardest parts of the job… I have started playing worship music on my headphones, just to hear God’s promises in my head.
“As the leader of the team, I look in the faces of the nurses and technicians, and there is a lot of fear and anxiety I see on those faces. My goal is to have more hope than fear,” said Parnell. “To block out the COVID noise and show that Jesus is around us all the time.”

Parnell said his goal is to bring more hope than fear to his health care staff as the pandemic progresses.
Parnell is no stranger to providing medical care in extreme situations as he has carried out medical mission work in Baja, Mexico, since 1998 and has served as the team leader for Lipscomb’s medical mission trip to City of Children in Baja since 2015. He is also involved with opening a clinic through the organization Baja Missions in El Zorrillo, Mexico, in fall of 2020, “something we’ve been dreaming about for a while and wouldn’t have been possible without the Lipscomb Baja-med trip,” he said.
A year or two ago, that mission team was provided a donation of more than 100 N-95 masks, far more than the team needed that year. So the rest were put in storage at the City of Children orphanage in Mexico, Parnell said.
But recently, Parnell remembered the storehouse of masks and worked with the City of Children to distribute those masks and gowns to partner medical providers in Mexico.
“Clearly God has put those masks to work now that dentists and the doctors in Mexico have protection,” Parnell said. “God continues to move and work despite all the sadness, fear and anxiety.”
James Parnell (’06) graduated from medical school at the University of Tennessee at Memphis. He did his residency training at Vanderbilt University Medical Center and continues as a clinical instructor of emergency medicine at Vanderbilt. He is also the vice president for the Tennessee chapter of the American Academy of Emergency Medicine.